Social Determinants of Health: When Health Care is More Than Just Medicine
February 25, 2020
CMS projects that national health spending in the United States (US) will reach almost $6 trillion by 2027.1 Can a focus on social risk improve health and moderate skyrocketing costs?
In 2016, the United States spent almost twice as much on health care as ten other developed, high-income countries.2 Yet, performance on many outcome measures was lower. Why? According to a White Paper by Veradigm™, social determinants of health (SDoH) lead to discrepancies between what we invest in and get out of our health care.
What are the Social Determinants of Health?
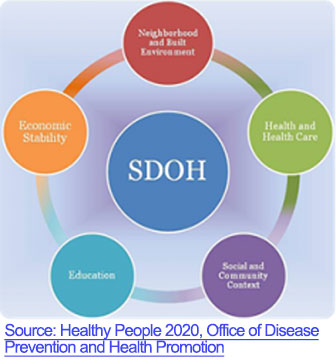
Social determinants of health are the single largest predictor of the health outcomes of a population.5 To improve health outcomes, SDoH factors such as economic instability, education, and social support need to be addressed.6 Addressing SDoH can impact everything from care utilization patterns (i.e., patients being seen in a primary care setting with lower costs rather than emergency room visits) to increased medication adherence and can lead to improved use of prevention strategies.7
Using SDoH to Improve Care and Reduce Cost
Providers and insurance plans can utilize SDoH data to gain valuable insights into the health status of their patient pools as well as identify “vulnerable” subgroups.8 This understanding could lead to better patient/provider communication as well, since a vast majority of patients in a national survey indicated that they wanted their healthcare providers to ask about their social needs.9 It isn’t sufficient to simply identify that unmet needs exist within a population. To fill those needs, we need to first determine what caused them.
A recent study conducted by Veradigm™ suggests that the use of a comprehensive approach which addresses the social, behavioral and environmental risk factors can lead to improved patient and population level outcomes, reductions in medical costs and eventually lead to value-based care.
What are the barriers to routine use of SDoH?
While some social determinants of health data can currently be obtained from electronic health records (EHRs), routine screening is infrequently conducted at the provider level for the five key social needs of a population.9 These five social determinant categories are:
- Economic stability;
- Education;
- Social and community context;
- Health and health care;
- Neighborhood and built environment.
Additionally, a lack of standard definitions for data collection as well as for use of information presents additional challenges.8
Real-World Example of How to Capture and Use Social Determinants of Health Data from EHRs
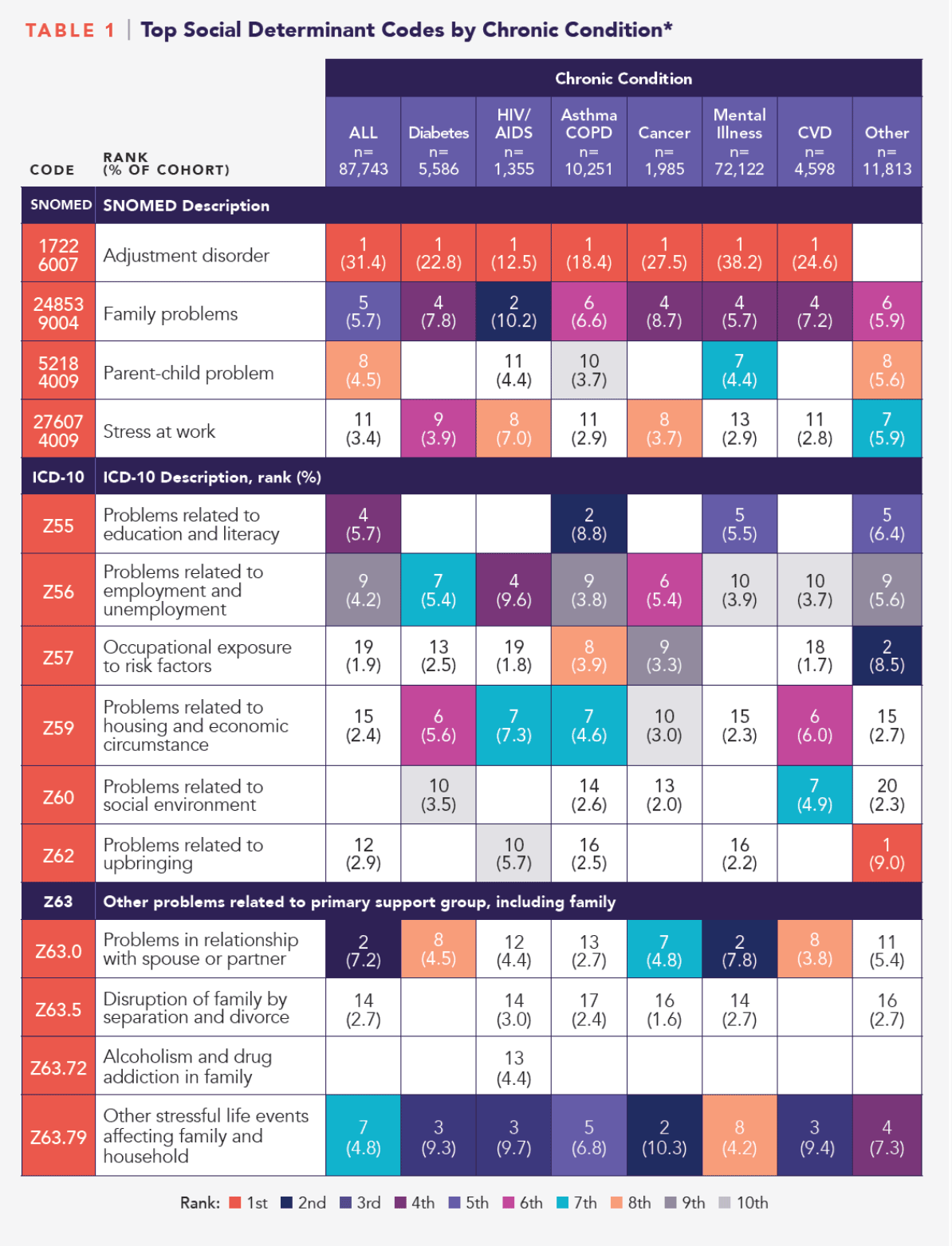
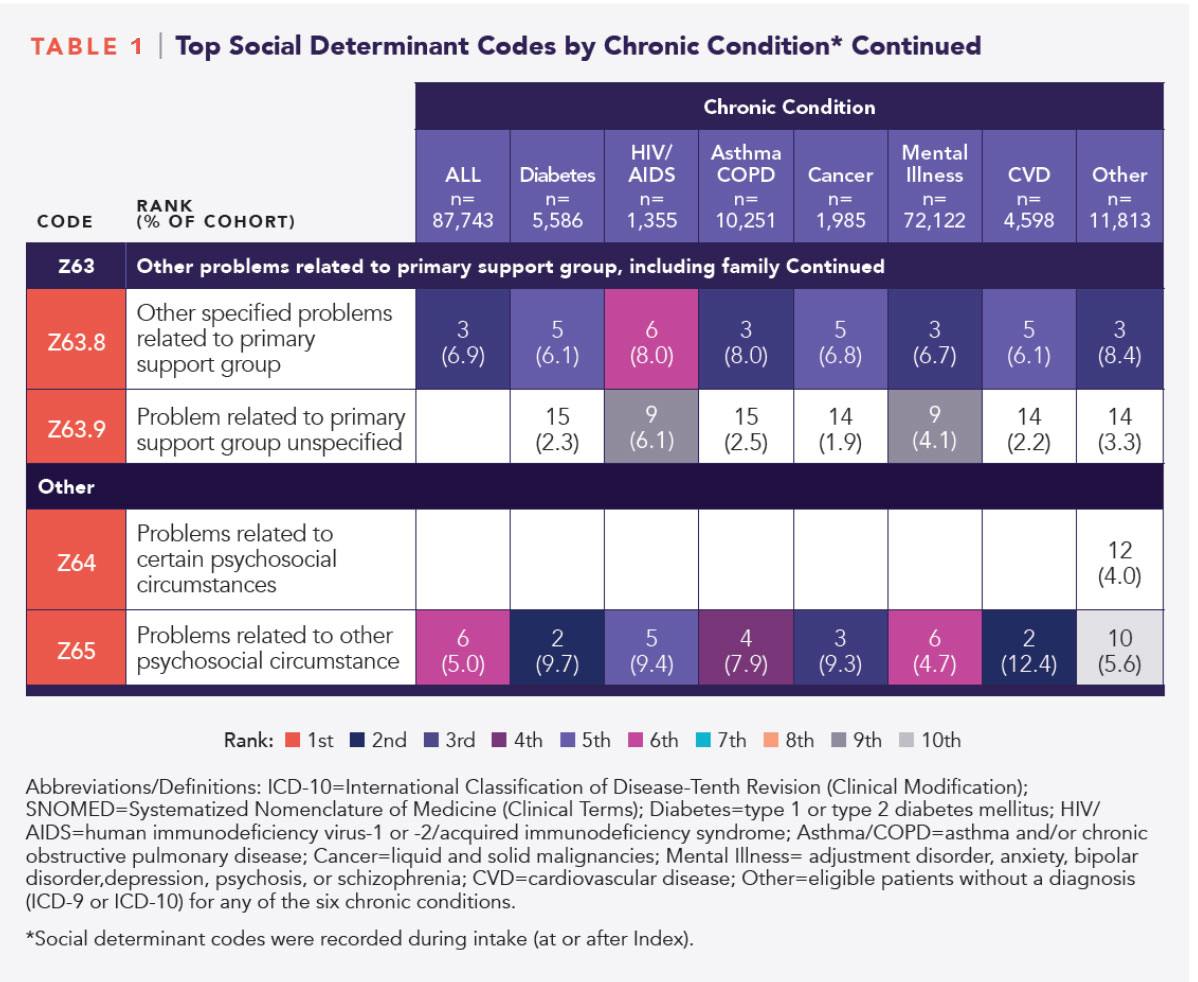
Among 75,930 patients, there were 95,897 chronic conditions recorded, with mental illness the most prevalent (82.2% of the sample). The majority (84%) of patients in each of the chronic condition cohorts were assigned social determinants codes by their primary care practitioners, most commonly Adjustment Disorder (SNOMED CT).
However, a sizable portion (13.5%) had social determinants codes but no diagnoses for the specified chronic conditions. This group of patients with no diagnoses highlights the utility of SDoH data. SDoH-related risk factors have been associated with increased risk of developing diabetes and hypertension. By implementing a comprehensive outreach program, this group’s risk could potentially be mitigated, yielding lowered morbidity and mortality long term. This table from the white paper shows the top social determinant codes by chronic condition.
Implications for the Future of Health Care
The results of the Veradigm™ retrospective cohort study indicate the potential to identify and fill gaps in the patient experience. For patients with demonstrated social risk, social determinant data captured together with clinical data may be assessed longitudinally using predictive analytics to help determine which patients might require more intensive social or clinical support to forestall the onset of chronic disease. While social determinant data are more routinely being collected in clinical care settings, lack of industry standards for data collection remains a significant issue; however, comprehensive coding frameworks that align definitions and the use of information technology tools such as natural language processing are being used to extract and standardize SDoH data from problem lists and EHR text fields.
Moreover, this study provided insight into treatment access and medication non-adherence. Nonadherence to medications presents a significant challenge to treatment and improving patient outcomes. Lack of affordability is a key reason why one in five patients are nonadherent.9 Interactive cloud-based platforms that provide EHR and evidence data along with SDoH variables can provide insight into barriers hindering treatment or contributing to non-adherence. EHRs may also host personalized care plans that incorporate social and clinical risks, identify resources, outline treatment goals, list medications with instructions for proper use, and provide instruction for self-management. And, they may provide literacy-level appropriate educational support tools that can be used for shared decision-making with respect to cost and treatment plans.
Conclusion
The life sciences industry is currently evaluating how social risk might be contextualized. As interactive, cloud-based platforms that securely manage comprehensive patient data and offer evidence-based tools, EHRs hold the potential to support the clinical, social, and educational needs of patients with chronic conditions and social risk. Studies that leverage real-world data from EHR platforms may provide incremental insight into treatment barriers, non-adherence, and other challenges encountered in caring for patients with complex health and social needs. For more information on next-generation data-driven insights and solutions, please visit https://veradigm.com.
[1] CMS. National Health Expenditure Projections 2018-2027.
[2] Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018; 319(10): 1024-1039.
[3] Centers for Disease Control and Prevention. Social determinants of health: know what affects health. Available at: https://www.cdc.gov/socialdeterminants/
[4] University of Wisconsin Population Health Institute. County health rankings key findings 2018. Available at: https://www.countyhealthrankings.org/reports/2018-county-health-rankings-key-findings-report
[5] County of Los Angeles Department of Public Health. Social Determinants of Health: How social and economic factors affect health. Available at: http://publichealth.lacounty.gov/epi/docs/SocialD_Final_Web.pdf
[6] McKinsey & Company. Addressing the social determinants of health: Capturing improved health outcomes and ROI for state Medicaid programs. Available at: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/addressing-the-social-determinants-of-health
[7] PWC. Top health industry issues of 2018. https://www.pwc.com/us/en/industries/health-industries/top-health-industry-issues/social-determinants.html
[8] eHealth Initiative. The importance of social determinants of health data. Available at: https://www.ehidc.org/sites/default/files/resources/files/Importance%20of%20SDOH%20Data%20March%202019.pdf
[9] Kaiser Permanent 2019. Survey: Housing, food, isolation major barriers to health. Available at: https://about.kaiserpermanente.org/community-health/news/survey-housing-food-isolation-major-barriers-to-health
[10] Patel MR et al. Social determinants of health, cost-related non-adherence, and cost-reducing behaviors among adult with diabetes: findings from the National Health Interview Survey. Med Care. 2016: 54(8): 796-803.