US Government Accountability Office Report on State-Directed Medicaid Payments in Managed Care
June 29, 2022
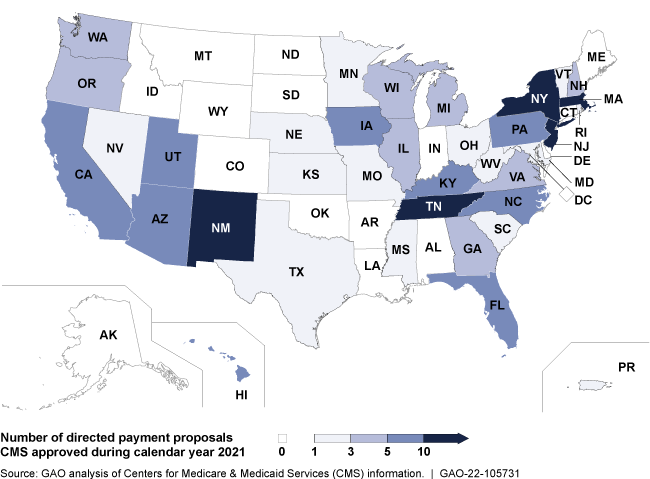
The US Government Accountability Office (GAO) released a new report on state-directed payments of Medicaid funds to managed care plans. Earlier this year, Medicaid approved nearly $20 billion in funding in proposals from states looking to direct funding to care providers that meet predetermined goals. However, states report estimated payments, not actual payments, so a gap in oversight exists.
According to the report, “CMS [Centers for Medicare & Medicaid Services] requires states to estimate the amount of directed payments prior to approval, but CMS does not have information on the actual amounts paid. In December 2020, GAO made a recommendation that if implemented would address some of the information gaps CMS faces. Specifically, GAO recommended CMS should collect and document complete and consistent provider-specific information about Medicaid payments to providers, including state directed payments. Doing so would likely improve CMS’s ability to identify potentially impermissible financing and payments for additional review. GAO plans to continue examining CMS’s oversight of these payments.”
To read more, click here.
(Source: US Government Accountability Office, June 28th, 2022)